Jun 22, 2020
States don't need new lockdowns to cut COVID spread
, Bloomberg News
Whether you call it a second wave or, more accurately, the easily foreseeable continuation of a pandemic, COVID-19 is still spreading unchecked in several American states. Florida, Arizona, Texas and other states are reporting record numbers of new cases.
And many are neglecting to take steps that could prevent outbreaks from expanding into possibly unmanageable surges in COVID-19 cases and deaths.
State leaders understandably resist the notion of issuing new stay-at-home orders, which would be painful, unpopular and at this point difficult to enforce. Lockdowns averted millions of potential cases in the spring, and they may still be required if case growth gets out of hand. But blunt quarantine isn’t the only way to check COVID-19.
Over the past several months, scientists worldwide have come to better understand how infections occur and what specific measures can most effectively prevent them. States can and should pay attention to what the experts have learned and use it to steer public behavior toward safety.
It won’t help to dismiss rising case counts as concentrated outbreaks or an illusion created by increased testing, as the governors of Texas and Florida did last week.
While hot spots account for some of the case growth, and testing is up, neither of these explain why the two states are seeing thousands of new infections every day. Case growth is widespread, and the percentage of tests coming back positive — a measure that indicates the level of uncontained community spread — is steadily rising.
In Texas and Arizona, current hospitalizations are ticking up.
The same may or may not be true in Florida, which inexcusably fails to report that data daily.
While governors are keen to note that hospitals have spare capacity, that advantage could disappear quickly. Hospital beds fill up faster than they empty, and COVID-19 doesn’t strike according to where beds are available. Also, as more beds and hospital staff must be devoted to COVID, other care gets pushed aside, with damaging results.
The most potentially reassuring news is that that the death rate from COVID-19 in the four states with the largest new outbreaks is holding steady.
This may be because of improving treatment, broader testing that catches cases early when they’re easier to manage, and widespread precautions that protect those most at risk, including the elderly.
On the other hand, it may simply reflect the fact that death rates are a lagging indicator. It takes time to develop a COVID infection severe enough to require intensive care, and the sickest patients often spend weeks on ventilators. Many of this week’s deaths stemmed from infections that happened last month.
A younger-skewing outbreak will result in fewer deaths in the near-term. However, each case represents an avenue of possible transmission to someone more at-risk, and scientists are still assessing the long term impact of infection on people of all ages.
Governors should understand that they can lower their case rates without locking down their economies if they pay attention to what experts have observed about COVID-19 contagion: Well-spaced outdoor activities appear to pose little risk.
People don’t seem to easily pick up the virus from food or surfaces that others have touched. But the disease spreads readily among people who engage in prolonged close contact in crowded and poorly ventilated spaces.
So it’s possible to limit transmission by restricting crowds and calling for social distancing indoors. People who stand just one meter (a little over three feet) away from others stand a drastically lower chance of infection than those who get closer, and the risk decreases further with greater distance.
Widespread use of masks in high-risk situations reduces the risk of infection still more. Mask mandates in 15 states may have prevented as many as 450,000 COVID cases in the U.S., a recent study reported in Health Affairs found.
Effective public health efforts to track new infections and trace and isolate the contacts of those infected can also lower the risk of infection in a population by more than half, new modeling from U.K.-based researchers suggests.
While such efforts are useful in stemming any infectious disease, they are especially so for one like COVID, which often produces no symptoms and transmits readily within homes.
The caveat is, the more virus there is circulating in a community, the harder it is to stay ahead of the spread with testing and contact tracing. Targeted suppression efforts take longer to work than broad lockdowns do. To avoid the need for new stay-at-home orders, in other words, states need a greater sense of urgency about taking more targeted steps.
Of course, most states, including those seeing rising case counts, recommend social distancing and maintain some capacity limits on retail businesses.
But widespread reports of careless behavior and renewed case growth suggest that either the rules are too lax or people just aren’t following them.
Clearly, it’s not enough to merely ask people to protect themselves. It takes effort and consistent communication to shift behavior enough to change transmission dynamics.
This is particularly true when it comes to masks, which have become politicized in the U.S. Covering your face before entering a grocery store is properly viewed as an easy way to protect yourself and others.
Unfortunately, neglecting this basic human courtesy has become a form of protest against government overreach.
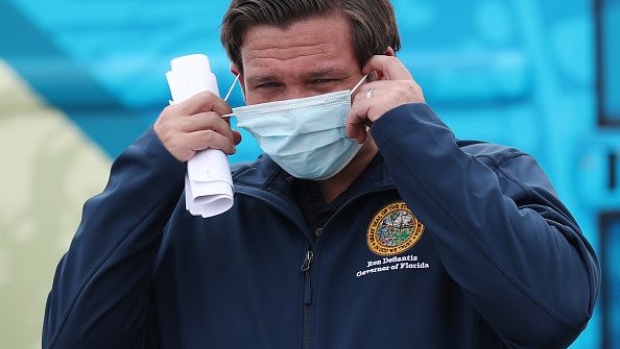
State leaders can and should try to discourage such protest — including by broadly mandating mask-wearing, as California Governor Gavin Newsom did last week.
Governors still dragging their feet on mask use seem not to care as much as they need to about saving lives. In the face of the country’s worst new COVID outbreak, Arizona Governor Doug Ducey has finally allowed local officials to require masks, but he’s still leaving policy up to individual communities.
Texas Governor Greg Abbott now allows local mask mandates, but only if officials impose them indirectly by placing rules on businesses, not people.
There are many ways in which state leaders can steer people toward safer behavior, bend their COVID-19 curves downward and strengthen their economies. It’s simply a matter of paying attention to how the coronavirus spreads.
This column does not necessarily reflect the opinion of the editorial board or Bloomberg LP and its owners.
Max Nisen is a Bloomberg Opinion columnist covering biotech, pharma and health care. He previously wrote about management and corporate strategy for Quartz and Business Insider.





